September 3, 2024
Reusable or Disposable? 10 Key Incontinence Care Considerations

Effective incontinence care prioritizes dignity while minimizing the exposure of a patient’s skin to moisture1. But, how do you know which underpad option is best for your patients? What are the differences between a reusable and a disposable underpad? Certain types of patients may be more likely to experience negative outcomes due to incontinence, including persons with limited mobility or with a reduced ability to reposition, as well as long-term care residents and patients over the age of 65.
Prolonged exposure to moisture from incontinence can create an environment for fungi, bacteria, or viruses which can lead to skin breakdown in the hospitalized patient or patients in care homes. Studies have shown this breakdown can begin within as little as 15 minutes of exposure. Preventive practices in incontinence care are important for patient health and well-being, but studies suggest that the quality of incontinence care varies2.
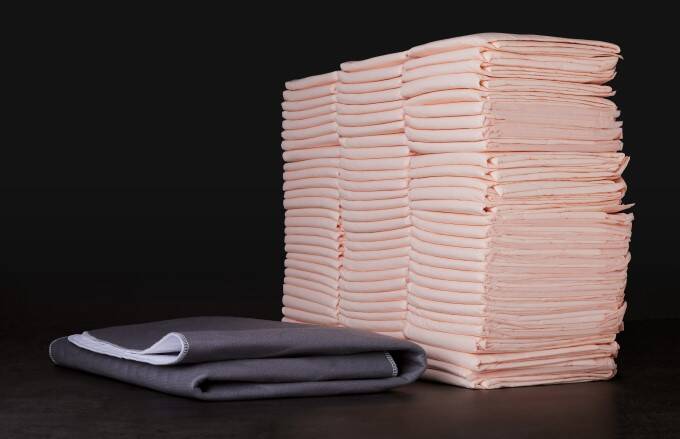
When it comes to choosing an underpad, some healthcare systems default to a disposable product. Disposable underpads do offer some clinical value, because they are effective at minimizing rewet and overall moisture management. However, disposables may also be perceived as a quick, use-and-toss bed protection item.
This choice to rely (or often over-rely) on disposable underpads misses critical opportunities for healthcare organizations to potentially improve patient experiences and outcomes, including the potential to reduce a patient’s length of stay and decrease the 30-day readmission rate. Proactive incontinence strategies can also help reduce supply costs and support environmental sustainability targets.
What is the difference between a disposable and a reusable incontinence pad?
Clinical experts agree that moisture control is essential for incontinence care. Moisture-associated damage to the skin’s barrier can lead to a variety of adverse symptoms, ranging from discomfort to serious infection, and it increases the potential for additional functional, physical, cognitive, and mobility issues in many patients.3 Therefore, both reusable and disposable underpads are designed to address moisture.
However, here are 10 important differences between the two options you may not be aware of:
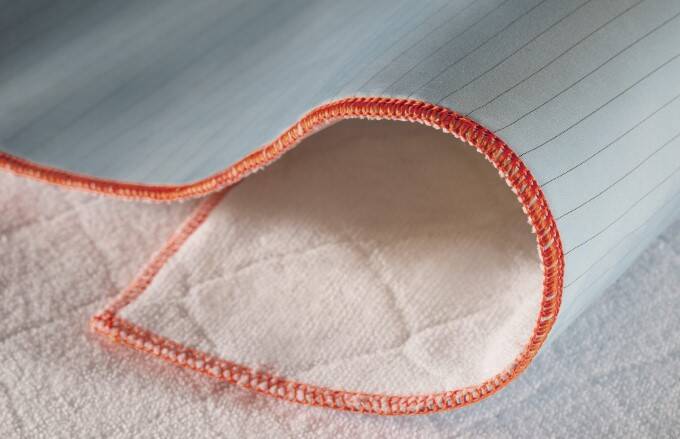
1. Clinical Benefits: Beyond fundamental moisture control, some reusable underpads provide actual clinical benefits to patients and contribute to improved patient outcomes. Many disposable underpads are designed to capture moisture in the center of the pad and hold the fluid within the interior polymers of the product4. Some reusable options, however, are engineered with an internal construction that absorbs moisture quickly and wicks it away from the center of the pad — and thus, away from the patient’s body.
2. Dry Time: A product that is fast drying is essential. Lightweight polyester blends found in many reusable underpads can provide a more comfortable patient experience. When enhanced with fibers that have built-in microchannels or moisture wicking chemistry, these pads dry faster than conventional cotton, paper, or plastic incontinence solutions.
3. Fluid Protection: In contrast to a paper or plastic-based disposable option, the multi-layered fabrication of some reusable underpad solutions may offer significantly enhanced protection from fluids, because of the focus on interior moisture management. For example, a reusable underpad with a hydrophobic top layer pulls liquid into the interior of the pad, away from the patient’s skin. The hydrophilic soaker layer facilitates movement of the liquid further into the product’s interior layers.
4. Strength: Reusable options with a soft, gentle facing surface tend toward greater overall strength and a much lower possibility of tearing when the product is repositioned beneath the patient. Some studies indicate that a reusable underpad can support effective repositioning up to 800 pounds, which may be more than double the weight capacity of a disposable product.
5. Friction and Shear: A reusable underpad can also reduce the potential for tearing force on the thinner skin that many patients (particularly elderly patients) may possess. Managing friction (the force of two surfaces rubbing against one another) and shear (the force of gravity between the patient and, in this case, the underpad) is essential for preventing pressure injury causes in incontinent patients.
6. Patient Dignity: The face fabrics of reusable underpads come in a variety of colors and/or patterns to help disguise incidental staining and increase patient dignity. In acute care or other settings where clinicians may not want the underpad to hide fluid color, reusable pad options are available in white-facing fabrics.
7. Waste Reduction: Many reusable items may be laundered and reused with no impact on absorbency or efficacy fifty or more times, leading to significant reductions in healthcare waste and supply costs over time.
8. Cost per Use: Costs differ when carefully evaluating a disposable versus reusable underpad options. In many cases, a reusable solution costs less over time, including laundering costs.
9. Environmental Footprint: A recently published study in the Journal of Nursing Care Quality explores a life cycle analysis of reusable underpads, including soiling, reusable cycles before removal, supply chains, laundry use, and end-of-life environmental impact. Findings indicate that the selection of reusable underpads versus disposables significantly reduced total natural resource energy consumption, greenhouse gas emissions, and blue water consumption.5
10. Sustainability: Healthcare facilities are the second highest contributor of environmental waste in the United States. The healthcare industry produces more than 6,600 tons of solid waste each day, which adds up to over four billion pounds of waste annually.6 The tangible costs to dispose of healthcare organizations’ solid waste continues to soar. Using reusable incontinence products reduces overall cost per use, reduces waste, and improves environmental sustainability efforts.7
Download infographic for a full summary
High-quality incontinence care is an important part of the healthcare experience. A healthcare system’s selection of the products used to support patient dignity should be part of ongoing value analysis conversations and carefully considered from multiple angles.
Have questions? Let’s connect.
Our team has been inspiring care, comfort, and change in our communities since 1940. We create the world’s most innovative textile solutions and help our customers use them in the most efficient way. To connect with our healthcare textile, clinical, and laundry experts, contact us today.
Related Content
Examining Environmental Footprints: Reusable and Disposable Incontinence Underpads
A recent study published in the Journal of Nursing Care Quality aims to support clinicians’ knowledge to include environmental sustainability in decisions regarding patient care and reusable versus disposable incontinence underpads. A life cycle analysis was conducted, including soiling, reusable cycles before removal, supply chains, laundry use, and end-of-life environmental impact.

Why Reusable Underpads? Talking Points for your Team
Equipping your team with more knowledge about reusable underpad solutions can help you determine the best approach for your facility.
Case Study: Moving to a Reusable Underpad System
With waste disposal costs rising and meticulous value analysis being increasingly important, one large U.S. hospital wanted to examine both patient experience and the cost-saving opportunities in switching to a reusable incontinence pad.