February 13, 2025
Why Reusable Underpads? Talking Points for your Team

Incorporating reusable incontinence care products into your facility may be an adjustment for your staff. However, as caretakers, your team recognizes that continuous improvement within healthcare must include strategic sustainability efforts and waste reduction.
The statistics are staggering. The healthcare industry produces more than 6,600 tons of solid waste every day, which adds up to over four billion pounds of waste annually. The tangible costs to dispose of healthcare organizations’ solid waste also continues to soar. Considering the impact of reusable incontinence pads is imperative.
Below are some important items to discuss with your staff as reusable incontinence pads are implemented into your system.
What are the benefits of a reusable underpad?
Experts agree that managing moisture and the microclimate around the patient’s skin is essential for attempting to prevent skin breakdown. Beyond fundamental moisture control, some reusable underpads provide actual clinical benefits to patients and contribute to improved patient outcomes. For example:
- Many disposable underpads are designed to capture moisture in the center of the pad and hold the fluid within the interior polymers of the product. Some reusable options, however, are engineered with an internal construction that absorbs moisture quickly and wicks it away from the center of the pad—and thus, away from the patient’s body.
- In contrast to a paper- or plastic-based disposable option, the multi-layered fabrication of some reusable underpad solutions may offer significantly enhanced protection from fluids, because of the focus on interior moisture management. For example, a reusable underpad with a hydrophobic top layer pulls liquid into the interior of the pad, away from the patient’s skin. The hydrophilic soaker layer facilitates movement of the liquid further into the product’s interior layers.
- A reusable underpad can reduce the potential for shearing force on the thinner skin that many patients (particularly elderly patients) are susceptible to. Managing friction (the force of two surfaces rubbing against one another) and shear (the force of gravity between the patient and, in this case, the underpad) is essential for preventing pressure injuries in incontinent patients.
- Reusable underpad options tend to provide greater overall strength and a much lower possibility of tearing when the product is used for repositioning patients.
- Reusable underpads tend to lie flatter under the patient and do not bunch up under the patient like disposable pads often do. This improves overall comfort and reduces pressure points on the patient’s skin. A reusable underpad that features rounded corners further reduces the potential for pressure points, and the corners’ construction prevents the pad from wrinkling or folding up underneath the patient’s body.
What are the sustainability and cost advantages of a reusable underpad?
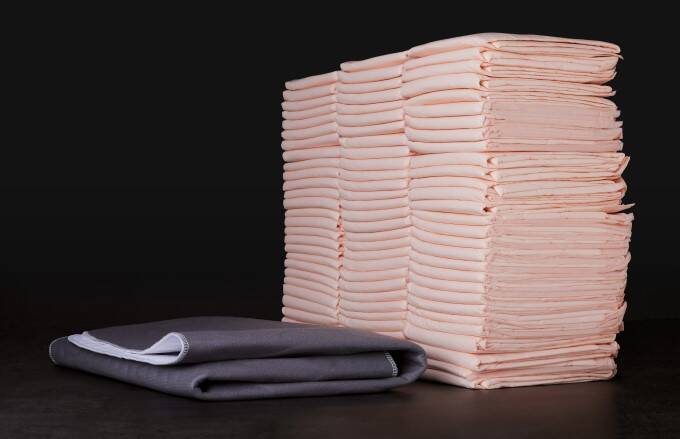
Disposable underpads generate tremendous amounts of waste.
- Clinicians are aware that there is a tendency to use more than one disposable pad below patients. Studies monitoring the usage patterns of disposable and reusable underpads indicate that on average, two disposable pads are used for every one reusable. Also, reusable incontinence pads do not require the use of draw sheets or flat sheets under the pad for patient repositioning. Eliminating these instances of over-use is a great step toward better sustainability and cost management.
- Disposable underpads are packaged in multiples of 5 or 10. Once a package is opened within the patient room, any unused pads are considered contaminated and are thrown out or sent home with patients— creating additional waste and expense.
- Significant supplies of disposable underpads need to be stocked and inventoried, taking up valuable storage space within facilities. Reusables can be maintained with appropriate par levels on a linen cart and quickly replenished as needed.
- A recently published study in the Journal of Nursing Care Quality explores a life cycle analysis of reusable underpads, including soiling, reusable cycles before removal, supply chains, laundry use, and end-of-life environmental impact. Findings indicate that the selection of reusable underpads versus disposables significantly reduced total natural resource energy consumption, greenhouse gas emissions, and blue water consumption.
- In many cases, a reusable solution has a lower cost per use (including laundering costs), resulting in a significantly lower total cost over time.
What are the best practices for using a reusable underpad?
Ongoing staff education about underpad utilization best practices is essential. Here are some general guidelines:
- Reusable incontinence pads can be used for incontinence care and patient positioning. Safe patient handling procedures should always be followed. Established protocols for incontinence patient care should always be followed. It is common to check for soiled underpads under the patient at least every two hours or as needed.
- Reusable incontinence pads do not require the use of draw sheets or flat sheets under the pad for patient repositioning. This eliminates a layer under the patient, which is beneficial for the patient’s microclimate. Only one reusable underpad should be placed under the patient for incontinence care.
- Underpads may be placed on the bed in either direction. If the pad is being utilized for patient positioning, it may be beneficial to place the underpads so that the longer side goes across the bed. This will provide the clinician with more material to grab when repositioning the patient.
- All soiled incontinence pads should be placed in the soiled linen bag (or hamper). This includes pads that are heavily soiled, stained with blood, or utilized for isolation patients.
- Follow standard infection control protocols when handling soiled underpads, including proper hand hygiene and disinfection of surfaces.
- Underpads should be stored in a designated stocking area/linen cart, away from contaminants and moisture.
- Only bring underpads into the patient’s room as needed. Excess unused linen in the patient room at the time of patient discharge is considered soiled and generates unnecessary waste and expense.
Preventive incontinence care practices are essential for patient health and well-being, and for helping to move healthcare systems along the path to greater sustainability. Equipping your team with more knowledge about reusable incontinence care solutions can help you determine the right approach for your facility.
We’re here to help. Our team has been inspiring care, comfort, and change in our communities since 1940. We can support your sustainability efforts, strengthen your supply, and help provide positive outcomes for your patients and staff. To connect with a member of our healthcare team of experts, contact us today.
Related Content

Reusable Underpads 101: Everything You Need to Know
Reusable underpads deliver numerous benefits over single-use disposable products. But how do they work? And what factors need to be considered when selecting an incontinence care solution?
Examining Environmental Footprints: Reusable and Disposable Incontinence Underpads
A recent study published in the Journal of Nursing Care Quality aims to support clinicians’ knowledge to include environmental sustainability in decisions regarding patient care and reusable versus disposable incontinence underpads. A life cycle analysis was conducted, including soiling, reusable cycles before removal, supply chains, laundry use, and end-of-life environmental impact.

Reusable or Disposable? 10 Key Incontinence Care Considerations
Effective incontinence care prioritizes dignity while minimizing the exposure of a patient’s skin to moisture. But, how do you know which underpad option is best for your patients? What are the differences between a reusable and a disposable underpad? Read our latest blog to learn more.